Abstract
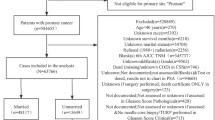
While being in a committed relationship is associated with a better prostate cancer prognosis, little is known about how marital status relates to its incidence. Social support provided by marriage/relationship could promote a healthy lifestyle and an increased healthcare seeking behavior. We investigated the association between marital status and prostate cancer risk using data from the PRACTICAL Consortium. Pooled analyses were conducted combining 12 case–control studies based on histologically-confirmed incident prostate cancers and controls with information on marital status prior to diagnosis/interview. Marital status was categorized as married/partner, separated/divorced, single, or widowed. Tumours with Gleason scores ≥ 8 defined high-grade cancers, and low-grade otherwise. NCI-SEER’s summary stages (local, regional, distant) indicated the extent of the cancer. Logistic regression was used to derive odds ratios (ORs) and 95% confidence intervals (CI) for the association between marital status and prostate cancer risk, adjusting for potential confounders. Overall, 14,760 cases and 12,019 controls contributed to analyses. Compared to men who were married/with a partner, widowed men had an OR of 1.19 (95% CI 1.03–1.35) of prostate cancer, with little difference between low- and high-grade tumours. Risk estimates among widowers were 1.14 (95% CI 0.97–1.34) for local, 1.53 (95% CI 1.22–1.92) for regional, and 1.56 (95% CI 1.05–2.32) for distant stage tumours. Single men had elevated risks of high-grade cancers. Our findings highlight elevated risks of incident prostate cancer among widowers, more often characterized by tumours that had spread beyond the prostate at the time of diagnosis. Social support interventions and closer medical follow-up in this sub-population are warranted.



Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy and ethical restrictions.
Code availability
Available from the authors on request.
References
International Agency for Research on Cancer. GLOBOCAN 2018, Estimated Incidence, mortality and prevalence of 36 cancer types in 185 countries 2018. http://gco.iarc.fr/. Accessed 29 Mar 2019.
Thun M, Linet MS, Cerhan JR, Haiman CA, Schottenfeld D. Cancer epidemiology and prevention. 4th ed. Oxford: Oxford University Press; 2017.
Conti DV, Darst BF, Moss LC, Saunders EJ, Sheng X, Chou A, et al. Trans-ancestry genome-wide association meta-analysis of prostate cancer identifies new susceptibility loci and informs genetic risk prediction. Nat Genet. 2021;53(1):65–75. https://doi.org/10.1038/s41588-020-00748-0.
Klassen AC, Platz EA. What can geography tell us about prostate cancer? Am J Prev Med. 2006;30(2 Suppl):S7-15. https://doi.org/10.1016/j.amepre.2005.09.004.
Loeb S, Drevin L, Robinson D, Holmberg E, Carlsson S, Lambe M, et al. Risk of localized and advanced prostate cancer among immigrants versus native-born Swedish men: a nation-wide population-based study. Cancer Causes Control. 2013;24(2):383–90. https://doi.org/10.1007/s10552-012-0124-6.
Mucci LA, Hjelmborg JB, Harris JR, Czene K, Havelick DJ, Scheike T, et al. Familial risk and heritability of cancer among twins in Nordic countries. JAMA. 2016;315(1):68–76. https://doi.org/10.1001/jama.2015.17703.
Verbrugge LM. Marital status and health. J Marriage Fam. 1979;41(2):267–85. https://doi.org/10.2307/351696.
Robards J, Evandrou M, Falkingham J, Vlachantoni A. Marital status, health and mortality. Maturitas. 2012;73(4):295–9. https://doi.org/10.1016/j.maturitas.2012.08.007.
Schoeppe S, Vandelanotte C, Rebar AL, Hayman M, Duncan MJ, Alley SJ. Do singles or couples live healthier lifestyles? Trends in Queensland between 2005–2014. PLoS ONE. 2018;13(2): e0192584. https://doi.org/10.1371/journal.pone.0192584.
Eng PM, Kawachi I, Fitzmaurice G, Rimm EB. Effects of marital transitions on changes in dietary and other health behaviours in US male health professionals. J Epidemiol Community Health. 2005;59(1):56–62. https://doi.org/10.1136/jech.2004.020073.
Teachman J. Body weight, marital status, and changes in marital status. J Fam Issues. 2016;37(1):74–96. https://doi.org/10.1177/0192513X13508404.
Pettee KK, Brach JS, Kriska AM, Boudreau R, Richardson CR, Colbert LH, et al. Influence of marital status on physical activity levels among older adults. Med Sci Sports Exerc. 2006;38(3):541–6. https://doi.org/10.1249/01.mss.0000191346.95244.f7.
Watt RG, Heilmann A, Sabbah W, Newton T, Chandola T, Aida J, et al. Social relationships and health related behaviors among older US adults. BMC Public Health. 2014;14(1):533. https://doi.org/10.1186/1471-2458-14-533.
Blumberg SJ, Vahratian A, Blumberg JH. Marriage, cohabitation, and men’s use of preventive health care services. NCHS Data Brief. 2014;154:1–8.
Stafford M, von Wagner C, Perman S, Taylor J, Kuh D, Sheringham J. Social connectedness and engagement in preventive health services: an analysis of data from a prospective cohort study. Lancet Public Health. 2018;3(9):e438–46. https://doi.org/10.1016/s2468-2667(18)30141-5.
Keating NL, O’Malley AJ, Murabito JM, Smith KP, Christakis NA. Minimal social network effects evident in cancer screening behavior. Cancer. 2011;117(13):3045–52. https://doi.org/10.1002/cncr.25849.
Meiser B, Cowan R, Costello A, Giles GG, Lindeman GJ, Gaff CL. Prostate cancer screening in men with a family history of prostate cancer: the role of partners in influencing men’s screening uptake. Urology. 2007;70(4):738–42. https://doi.org/10.1016/j.urology.2007.06.1093.
Tyson MD, Andrews PE, Etzioni DA, Ferrigni RG, Humphreys MR, Swanson SK, et al. Marital status and prostate cancer outcomes. Can J Urol. 2013;20(2):6702–6.
Aizer AA, Chen MH, McCarthy EP, Mendu ML, Koo S, Wilhite TJ, et al. Marital status and survival in patients with cancer. J Clin Oncol. 2013;31(31):3869–76. https://doi.org/10.1200/jco.2013.49.6489.
Knipper S, Preisser F, Mazzone E, Mistretta FA, Palumbo C, Tian Z, et al. Contemporary analysis of the effect of marital status on survival of prostate cancer patients across all stages: a population-based study. Urol Oncol. 2019. https://doi.org/10.1016/j.urolonc.2019.04.023.
Lehrer S, Rosenzweig KE. Being a widower may be an indication for routine prostate-specific antigen screening above age 69 years, which the American Urological Association recommends as a cutoff point. Cancer. 2016;122(16):2604. https://doi.org/10.1002/cncr.30098.
Andersson SO, Baron J, Bergström R, Lindgren C, Wolk A, Adami HO. Lifestyle factors and prostate cancer risk: a case-control study in Sweden. Cancer Epidemiol Biomark Prev. 1996;5(7):509–13.
Cox B, Sneyd MJ, Paul C, Skegg DC. Risk factors for prostate cancer: a national case-control study. Int J Cancer. 2006;119(7):1690–4. https://doi.org/10.1002/ijc.22022.
Fincham SM, Hill GB, Hanson J, Wijayasinghe C. Epidemiology of prostatic cancer: a case-control study. Prostate. 1990;17(3):189–206.
Harvei S, Kravdal O. The importance of marital and socioeconomic status in incidence and survival of prostate cancer. An analysis of complete Norwegian birth cohorts. Prev Med. 1997;26(5 Pt 1):623–32.
Hayes RB, de Jong FH, Raatgever J, Bogdanovicz J, Schroeder FH, van der Maas P, et al. Physical characteristics and factors related to sexual development and behaviour and the risk for prostatic cancer. Eur J Cancer Prev. 1992;1(3):239–45.
La Vecchia C, Franceschi S, Talamini R, Negri E, Boyle P, D’Avanzo B. Marital status, indicators of sexual activity and prostatic cancer. J Epidemiol Community Health. 1993;47(6):450–3.
Lund Nilsen TI, Johnsen R, Vatten LJ. Socio-economic and lifestyle factors associated with the risk of prostate cancer. Br J Cancer. 2000;82(7):1358–63. https://doi.org/10.1054/bjoc.1999.1105.
Meijer M, Bloomfield K, Engholm G. Neighbourhoods matter too: the association between neighbourhood socioeconomic position, population density and breast, prostate and lung cancer incidence in Denmark between 2004 and 2008. J Epidemiol Community Health. 2013;67(1):6–13. https://doi.org/10.1136/jech-2011-200192.
Newell GR, Pollack ES, Spitz MR, Sider JG, Fueger JJ. Incidence of prostate cancer and marital status. J Natl Cancer Inst. 1987;79(2):259–62.
Randi G, Altieri A, Gallus S, Chatenoud L, Montella M, Franceschi S, et al. Marital status and cancer risk in Italy. Prev Med. 2004;38(5):523–8. https://doi.org/10.1016/j.ypmed.2003.12.004.
Wiren SM, Drevin LI, Carlsson SV, Akre O, Holmberg EC, Robinson DE, et al. Fatherhood status and risk of prostate cancer: nationwide, population-based case-control study. Int J Cancer. 2013;133(4):937–43. https://doi.org/10.1002/ijc.28057.
Penney KL, Stampfer MJ, Jahn JL, Sinnott JA, Flavin R, Rider JR, et al. Gleason grade progression is uncommon. Cancer Res. 2013;73(16):5163–8. https://doi.org/10.1158/0008-5472.CAN-13-0427.
Hurwitz LM, Agalliu I, Albanes D, Barry KH, Berndt SI, Cai Q, et al. Recommended definitions of aggressive prostate cancer for etiologic epidemiologic research. J Natl Cancer Inst. 2021. https://doi.org/10.1093/jnci/djaa154.
Wright JL, Salinas CA, Lin DW, Kolb S, Koopmeiners J, Feng Z, et al. Prostate cancer specific mortality and Gleason 7 disease differences in prostate cancer outcomes between cases with Gleason 4 + 3 and Gleason 3 + 4 tumors in a population based cohort. J Urol. 2009;182(6):2702–7. https://doi.org/10.1016/j.juro.2009.08.026.
Ruhl J, Callaghan C, Hurlbut A, Ries L, Adamo P, Dickie L, et al. Summary stage 2018: codes and coding instructions. Bethesda: National Cancer Institute; 2018.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377–99. https://doi.org/10.1002/sim.4067.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–74. https://doi.org/10.7326/m16-2607.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration. 2011.
Buja A, Lago L, Lago S, Vinelli A, Zanardo C, Baldo V. Marital status and stage of cancer at diagnosis: a systematic review. Eur J Cancer Care. 2018;27:e12755. https://doi.org/10.1111/ecc.12755.
Umberson D, Crosnoe R, Reczek C. Social Relationships and Health behavior across life course. Annu Rev Sociol. 2010;36:139–57. https://doi.org/10.1146/annurev-soc-070308-120011.
Cohen S. Social relationships and health. Am Psychol. 2004;59(8):676–84. https://doi.org/10.1037/0003-066x.59.8.676.
Sullivan AR, Fenelon A. Patterns of widowhood mortality. J Gerontol B Psychol Sci Soc Sci. 2014;69(1):53–62. https://doi.org/10.1093/geronb/gbt079.
Thierry X. Risks of mortality and excess mortality during the first ten years of widowhood. Population. 2000:81–109.
Norcross WA, Ramirez C, Palinkas LA. The influence of women on the health care-seeking behavior of men. J Fam Pract. 1996;43(5):475–80.
Tangen CM, Goodman PJ, Till C, Schenk JM, Lucia MS, Thompson IM Jr. Biases in recommendations for and acceptance of prostate biopsy significantly affect assessment of prostate cancer risk factors: results from two large randomized clinical trials. J Clin Oncol. 2016;34(36):4338–44. https://doi.org/10.1200/jco.2016.68.1965.
VanderWeele DJ, Brown CD, Taxy JB, Gillard M, Hatcher DM, Tom WR, et al. Low-grade prostate cancer diverges early from high grade and metastatic disease. Cancer Sci. 2014;105(8):1079–85. https://doi.org/10.1111/cas.12460.
Demoury C, Karakiewicz P, Parent ME. Association between lifetime alcohol consumption and prostate cancer risk: a case-control study in Montreal. Canada Cancer Epidemiol. 2016;45:11–7. https://doi.org/10.1016/j.canep.2016.09.004.
World Cancer Research Fund International/American Institute for Cancer Research. Continuous Update Project Report: Diet, Nutrition, Physical Activity, and Prostate Cancer. 2014.
Acknowledgements
The PRACTICAL consortium. This work was supported by the Canadian Institutes of Health Research, European Commission's Seventh Framework Programme Grant Agreement No. 223175 (HEALTH-F2-2009-223175), Cancer Research UK Grants C5047/A7357, C1287/A10118, C1287/A16563, C5047/A3354, C5047/A10692, C16913/A6135, and The National Institute of Health (NIH) Cancer Post-Cancer GWAS initiative Grant: No. 1 U19 CA 148537-01 (the GAME-ON initiative). We would also like to thank the following for funding support: The Institute of Cancer Research and The Everyman Campaign, The Prostate Cancer Research Foundation, Prostate Research Campaign UK (now PCUK), The Orchid Cancer Appeal, Rosetrees Trust, The National Cancer Research Network UK, The National Cancer Research Institute (NCRI) UK. We are grateful for support of NIHR funding to the NIHR Biomedical Research Centre at The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust. The Prostate Cancer Program of Cancer Council Victoria also acknowledge grant support from The National Health and Medical Research Council, Australia (126402, 209057, 251533, 396414, 450104, 504700, 504702, 504715, 623204, 940394, 614296), VicHealth, Cancer Council Victoria, The Prostate Cancer Foundation of Australia, The Whitten Foundation, PricewaterhouseCoopers, and Tattersall’s. EAO, DMK, and EMK acknowledge the Intramural Program of the National Human Genome Research Institute for their support. CS is the recipient of a doctoral fellowship from the Fonds de recherche du Québec - Santé. Additional funding and acknowledgments from individual studies in PRACTICAL are provided in supplementary materials.
Author information
Authors and Affiliations
Consortia
Contributions
CS conducted the analysis and prepared the manuscript. MEP supervised the work, participated in the conception of the study, and reviewed the manuscript. All authors participated in the interpretation of data, and provided important intellectual contributions to the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All individual studies were approved by local ethics committees and adhered to the principles of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional members from the PRACTICAL consortium are provided in the Supplementary Material. Information on the consortium can be found at http://practical.icr.ac.uk/.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Salmon, C., Song, L., Muir, K. et al. Marital status and prostate cancer incidence: a pooled analysis of 12 case–control studies from the PRACTICAL consortium. Eur J Epidemiol 36, 913–925 (2021). https://doi.org/10.1007/s10654-021-00781-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-021-00781-1