-
Cardiovascular
Peripheral artery disease can signal cardiovascular trouble for heart, brain and legs
If you have not heard of peripheral artery disease, or PAD, you are not alone. While clinicians and health organizations have made headway in raising awareness that heart disease is the No. 1 cause of death worldwide, PAD — despite being part of cardiovascular disease — is not as well-known.
PAD affects 8–10 million people in the U.S., most over the age of 65. But it also affects younger people who have additional risk factors, such as diabetes, smoking, obesity, and high blood pressure.
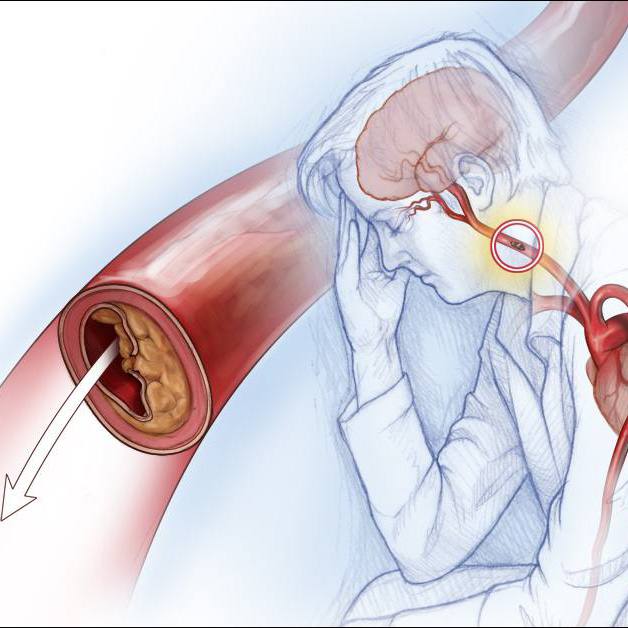
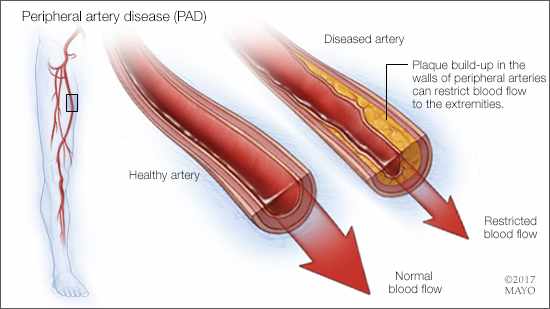
Peripheral artery disease involves the lower limbs, but it has its basis in atherosclerosis — a vascular disease where cholesterol plaque builds up in artery walls. This narrows the arteries, restricting circulation and possibly resulting in plaque breaking loose and forming a blood clot. Most patients with PAD will have vascular disease in more than one defined area, increasing the chances of serious complications.
Watch: Dr. Amy Pollak talks about peripheral artery disease.
Journalists: Broadcast-quality soundbites are available in the downloads at the bottom of the post. Please courtesy: "Mayo Clinic News Network." Read the script.
Unfortunately, peripheral artery disease has not traditionally been diagnosed early enough, and patients are often not treated with the most aggressive therapies. Addressing the issue of awareness and education in clinicians and patients is a key focus area in the new PAD National Action Plan spearheaded by the American Heart Association. This plan was developed in collaboration with 25 organizations and national leaders.
Dr. Amy Pollak, a Mayo Clinic cardiologist, co-chairs the effort to bring the plan to fruition, along with Dr. Aruna Pradhan of Brigham and Women's Hospital and Dr. Naomi Hamburg of Boston Medical Center.
The plan outlines goals to:
- Increase awareness of PAD for patients and health care providers
- Improve detection, treatment and ultimately health outcomes
- Reduce amputations related to peripheral artery disease through public health initiatives
- Increase and sustain research
- Advance advocacy efforts
"Lower-extremity PAD has not been prioritized the same way as cardiovascular disease or stroke. But there are several important points to consider," says Dr. Pollak. "If you have polyvascular disease — meaning cholesterol buildup that affects more than one area of the body, such as the heart, brain or leg — then you are at very high risk of heart attack, stroke, death or limb loss related to amputation. Patients with polyvascular disease and diabetes are at the highest PAD risk. We must ask about symptoms, treat these patients with aggressive medical therapy and follow them more closely."
Awareness and health disparities
Awareness is important because it opens the door to discuss prevention and treatment. Dr. Pollak notes that within the area of cardiovascular disease, the prevalence of PAD in the American population far surpasses all other types of cardiovascular and circulatory diseases, such as ischemic heart disease, stroke or atrial fibrillation.
"The American Heart Association did a survey that found that around 90% of people were aware of heart attack and stroke risks. But even in this group educated about heart disease and stroke, most people had not heard of PAD," says Dr. Pollak. "They did not know that you could have cholesterol buildup that involved blood vessels to your leg that could impact your ability to walk and be associated with limb loss. There are critical health disparities in patient education that we need to address because Black Americans are less aware of PAD."
Thirty percent of Black Americans will develop PAD, compared to 20% of non-Hispanic white Americans. Hispanic people and Native Americans have a similar 20% prevalence of PAD, but they tend to be diagnosed at a later stage of the disease.
The effects of health disparities regarding peripheral artery disease in Black Americans are stark. These patients often have more severe disease due to later diagnosis and are less likely to receive the best medical therapy. They have a higher risk of death due to cardiovascular events, such as a heart attack or stroke.
Black Americans are less likely to have procedures such as revascularization that can salvage a circulation-damaged limb. In turn, this leads to more nontraumatic amputations. The rate of amputations due to peripheral artery disease is markedly higher in the Southeast and Texas than the rest of the U.S.
Symptoms and diagnosis of PAD
As arteries leading to the legs develop significant cholesterol buildup that restricts blood flow, symptoms of PAD may appear. Some symptoms, such as lower leg cramps when walking, may be mild, severe or somewhere in between, but worsen as the disease progresses. Other symptoms may involve changes in the legs, such as coldness in one leg but not the other; shiny skin on the legs; slow growth of toenails and leg hair; sores on toes, feet or legs that do not heal; and no pulse or a weak pulse in legs. People may think some of these symptoms are just signs of aging, so it is important to address them with a health care professional. The most common symptom of PAD is a decreased ability to walk. Patients with PAD may not have any pain.
"We know that a history of tobacco use, or diabetes, are major risk factors for developing PAD. Other traditional risk factors, such as high blood pressure, high cholesterol and age, also increase the risk of PAD. We need to ask our patients with these risk factors if they have any symptoms that could be related to PAD and check their pulses in their feet. If they have concerning symptoms or an abnormal pulse exam, the next step is often doing a noninvasive ABI (ankle-brachial index) test," Dr. Pollak explains.
A physical exam can uncover symptoms that a patient may not be aware of or had simply attributed to something else. Dr. Pollak says it is important to remove socks and check the legs and feet of patients who fit the risk profile, even if they are younger. Clinicians can ask patients what sort of activities they can comfortably do to identify problems. And blood tests to check for diabetes and measure cholesterol also should be up to date.
Diagnostic tests, such as the ankle-brachial index test that compares blood pressure in a patient's ankle to that in their arm before and after exercise, can identify circulation issues in the legs. This test is a noninvasive way to identify the presence and severity of peripheral artery disease.
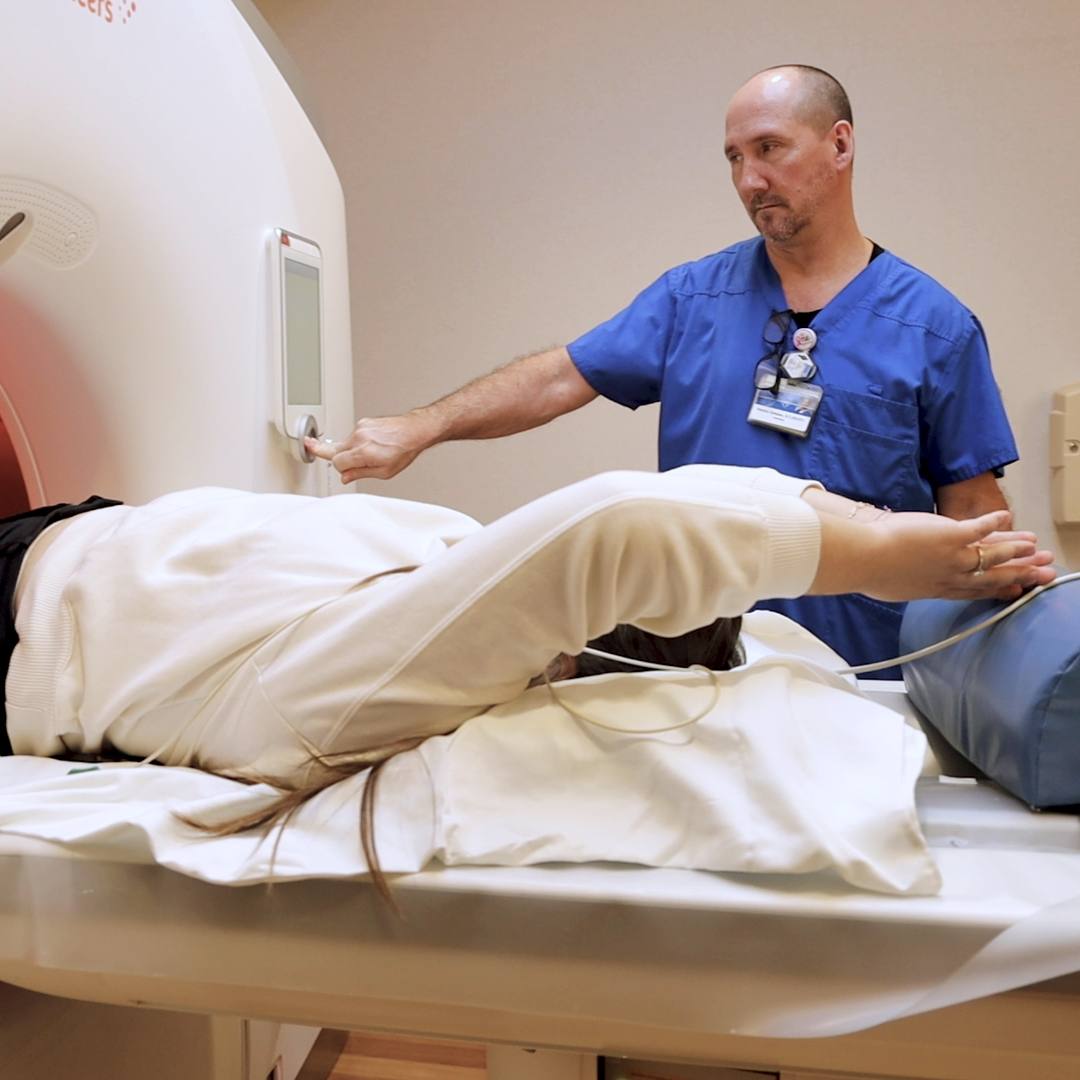
Angiograms use imaging technologies to home in on blockages and can be done with CTs or MRI. Catheter angiograms allow for treatment to open the arteries at the same time. When initiated early enough, revascularization in lower limbs restores blood flow and prevents the need for amputation. Losing mobility can affect a person's ability to work, making it more difficult to stay active and independent.
The stakes are high for patients and the health care system that cares for them. Approximately one-third of patients will die within five years of a peripheral artery disease diagnosis, and 20% will experience a heart attack or stroke.
"As a higher percentage of the U.S. population becomes older in the coming decades, progressive cardiovascular diseases like PAD will be relevant to even more people," notes Dr. Pollak. "Improving awareness, diagnosis and guideline-based treatment of PAD by 2025 is a crucial step to improve cardiovascular health and reduce nontraumatic amputations in the future."